Plantar fasciitis is such a problem that you can hardly conduct an image search for plantar fascia without returning mostly images of the plantar fascia with a big angry red splotch on the plantar fascia near the heel.
I recently watched a video on Facebook posted by one of my Physical Therapy peers on the topic of plantar fasciitis. I privately messaged him to let him know that I thought his presentation had missed some key points and his reply cited the Clinical Practice Guidelines for plantar fasciitis. There are some issues with that response from my standpoint:
1. The Clinical Practice Guidelines for plantar fasciitis are fairly useless in regards to “what to do” to treat plantar fasciitis and of some limited value in “what not to do”. They very accurately reflect current available research which is of little clinical value in this instance.
2. I’m concerned that my profession is so entranced by Evidence Based Practice (EBP) that they have stopped seeking information or guidance outside of what research has generated, and as a result their patients often suffer through suboptimal care and (pun intended) limp down the clinical plank of failed conservative care, injection and ill-advised surgery. I know this not what the developers of EBP-theory intended, but I’ve seen it just about daily on social media.
3. The research available on this topic is doing very little to help clinicians truly heal their patients of their foot pain. I would dearly love to pitch research ideas for anyone who has faculty connections.
Now off the Soap Box and on to clinical guidance…
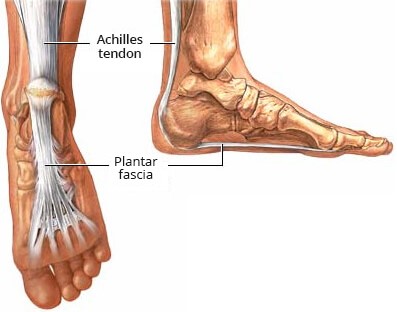
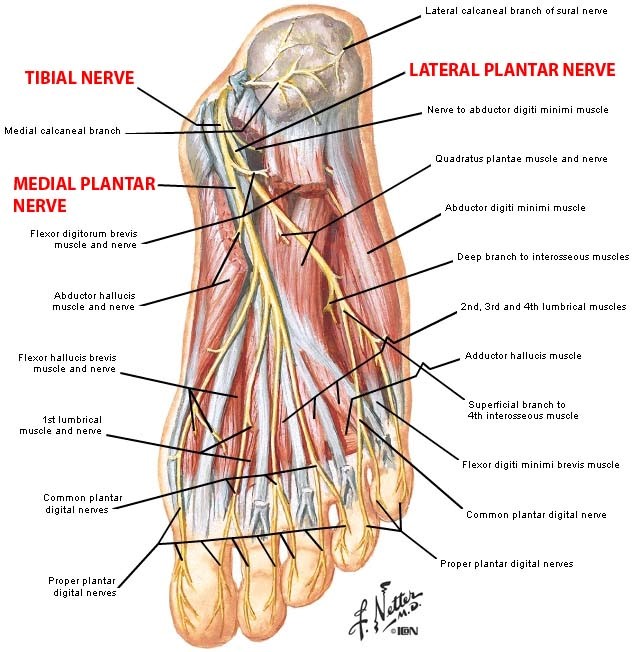
– Plantar fasciitis is a misnomer, most of these patients don’t use their plantar fascia at all. A more appropriate term would be “Mechanical Heel Pain”. Typically, the origin of Mechanical Heel Pain is a poor initial contact in stance phase in which the contact is too medial in magnitude and/or duration. The medial aspect of the midtarsal joint, subtalar joint and calcaneus are very neural dense and do not tolerate this increased pressure well and eventually leads to heel/foot pain.
– Unfortunately, a bad initial contact (as described above), has consequences throughout the foot and lower extremity that further perpetuate an inefficient gait cycle. Here are some examples: hallux abductovalgus (painful bunion), metatarsalgia, achilles tendinitis, medial knee pain (pes anserine, plica, etc), lateral hip pain (trochanteric bursitis, piriformis syndrome, etc) and SI dysfunction.
– The good news is that when you treat the cause (improve foot mechanics) and treat the tissue (manual therapy), the patients’ symptoms resolve very quickly…1-4 visits.
If you are a clinician reading this blog and you didn’t delete it from your feed after reading #2 above, you have practiced long enough to be frustrated at heel and foot pain patients’ poor prognoses. Please consider attending a lower extremity biomechanical course, it will completely change your practice. I teach a 2 day course called Thinking on Your Feet. Of course, I’m biased and think mine is best, but there are some other good courses out there. Give one of them a chance and it will elevate your practice above the limitations of the current Clinical Practice Guidelines.
If you are a patient reading this blog, you may have had “mainstream” care for your foot pain which probably included: activity modification, exercises (strengthening/stretching), modalities (heat, ice, ultrasound), massage, shoe inserts, dry needling, injections or surgery. You have probably been nodding your head the whole time, because you know your foot pain isn’t completely (or any) better. Find a clinician with biomechanical training in this topic or contact me directly for advice at Tony@BarePT.com or find out more about my unique practice and skill set at Barephysicaltherapy.com
LTC Tony Bare (ret) DPT, ATC, OCS
Laramie, WY
I had plantar fasciitis years ago. Had ultrasound don on the bottom of my foot about 6 times. It went away and has never bothered me since. I broke 2 bones in my foot and walked on it 9 months before 1 of 3 doctors I talked to about the foot pain finally took an xray. Only because I demanded it. Now I have constant pain on the top of my foot AND the plantar fasciitis is back with a vengeance! I get cortisone shots in the top of my foot every 6 months. It helps with the pain from the breaks, but not the PF. I’m to the point where I can barely walk because the pain is so bad. No one seems to want to try anything to help me! I now have bursitis in both sides of my upper thighs. I’ve had both knees replaced because I have arthritis in nearly every joint. My knees were so bad for years, but I had to wait until I was 60 to get them done. I’m 70 now. But my foot is causing me the most pain and I feel like it’s destroying my life. In the last 6 months, I’ve had to stop all activities because the PF is causing me so much pain. I’ve always had a very high tolerance of pain, but this is putting me DOWN! The pain in my foot is a 10 ALL the time. What can I do?!
LikeLike
Hi Belinda, just cleaning up some old posts from the website and ran across yours. Did my office manager reply to you? Are you now doing well? Please feel free to call me with any questions you might have.
Tony 3074140352
LikeLike